In partnership with the Montana Department of Public Health and Human Services and the Montana Public Health Institute, we are working with communities across the state to build effective behavioral health crisis response systems.
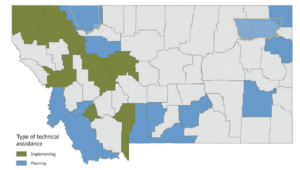
Through our Behavioral Health Continuum of Care Initiative, we support communities across the state to plan and implement the Crisis Now Model. Along with the Montana Department of Public Health and Human Services crisis diversion grants, we provide grants and technical assistance to support community planning, development, and implementation of the Crisis Now Model.
When a person experiences a behavioral health crisis such as an overdose, suicide attempt, or other mental health emergency, they are often brought by ambulance or law enforcement to the emergency department or jail. This approach is expensive, strains emergency and law enforcement resources, and can contribute to worse health outcomes.
Nationally, patients with behavioral health issues account for as many as one in four emergency department visits, resulting in estimated potentially avoidable costs of $4.6 billion each year. (source)
So far, 18 counties and two tribes are working on their crisis systems.
In 2022, seven counties established mobile crisis response teams and served more than 1,000 individuals.
Read our 2022 Annual Report for more highlights!
Learn More
Our Approach
The new crisis response systems in Montana are based on a national, best-practice model called Crisis Now. This model is designed to provide people in crisis with effective, appropriate care and avoid unnecessary use of emergency medical services and law enforcement.
The Crisis Now Model is well-suited for Montana because it is flexible and can be adapted to work successfully in urban, Native, and rural communities. The model has three components:
- Someone to Call: The 988 Suicide and Crisis Lifeline provides 24-hour support and care coordination over the phone. Most problems can be resolved by the call center’s crisis counselors.
- Someone to Respond: When a person needs more support, a centrally deployed crisis response team staffed by behavioral health professionals travels to the person to provide care, minimizing the impact on emergency medical services or law enforcement involvement.
- Somewhere to Go: A 24/7 crisis center offers safe, supportive care for people who cannot be stabilized by the crisis response team. These community-based facilities provide people in crisis with rapid, short-term assessment and treatment in a calm, therapeutic environment.
Behavioral Health System Progress
Efforts to implement the Crisis Now Model are still at an early stage in many communities. The ones that have begun are already seeing significant drops in behavioral health-related ER admissions and incarcerations.
So far, 18 counties and two tribes are working on their crisis systems. In 2022, seven counties established mobile crisis response teams and have collectively served more than 1,000 individuals.
Each county and tribe works with health care providers, law enforcement, behavioral health professionals, and other partners to customize and develop their crisis services according to their needs and resources. Here are two examples of what they are doing:
 LINCOLN COUNTY
LINCOLN COUNTY
Lincoln County operates an on-call shift system with half a dozen therapists from local communities who triage and respond to calls, either in person or through a phone consultation. A care coordinator follows up with callers to make sure they get any additional support they may need. This system makes efficient use of Lincoln County’s limited human resources. The number of behavioral health-related incarcerations, which used to range from eight to 15 a year, fell to just three in 2022.
 MISSOULA COUNTY
MISSOULA COUNTY
The Missoula Fire Department manages and operates Missoula’s mobile crisis response team. This co-responder model includes a licensed clinical social worker or counselor and an emergency medical technician employed by the fire department. As the state’s first fully operational mobile crisis response team, Missoula’s crisis response team currently responds to about 200 calls a month.
Our Support
We are currently offering grant funding to support communities interested in redesigning their crisis systems. Our support will help communities develop coalitions, complete system mapping to align behavioral health and criminal justice system resources, implement strategies to respond to behavioral health crises more effectively, and identify sustainable crisis funding sources. Regional collaboratives are prioritized.
All funding is by invitation only.
Contact
If you have a question about this initiative,
please email our program team.